November 10 is World Keratoconus Day. Keratoconus is a visual disorder you may well never have heard of, unless you happen to have it yourself. In which case, you will know just how challenging this degenerative condition can be.
In my case, I found that at the age of about 16 my sight was suddenly worsening rapidly. At first, I was treated simply for myopia (short sightedness). It was almost a year later that it became clear there was a more serious problem. I was diagnosed with keratoconus in one eye and told that glasses would no longer be sufficient for correcting my vision.
Keratoconus distorts the eye’s surface, the cornea. There are treatments available, especially if diagnosis is early, but no cure. It is usually first diagnosed in teenage patients who present with sight issues as their cornea begins to distort into a cone shape. This quickly results in severe myopia and irregular astigmatism (scattering).
Understanding the optics of keratoconus
It is difficult to imagine how these two symptoms combine and affect vision for someone who does not have the condition. So in support of World Keratoconus Day, I’d like to share exactly what it means for patients. I can do this thanks to the fact that we have recently conducted an internal R&D project to help understand the optics of keratoconus, its diagnosis, and how treatment can be improved. The results have been extremely interesting, with potential to be a real gamechanger in the treatment of the disease.
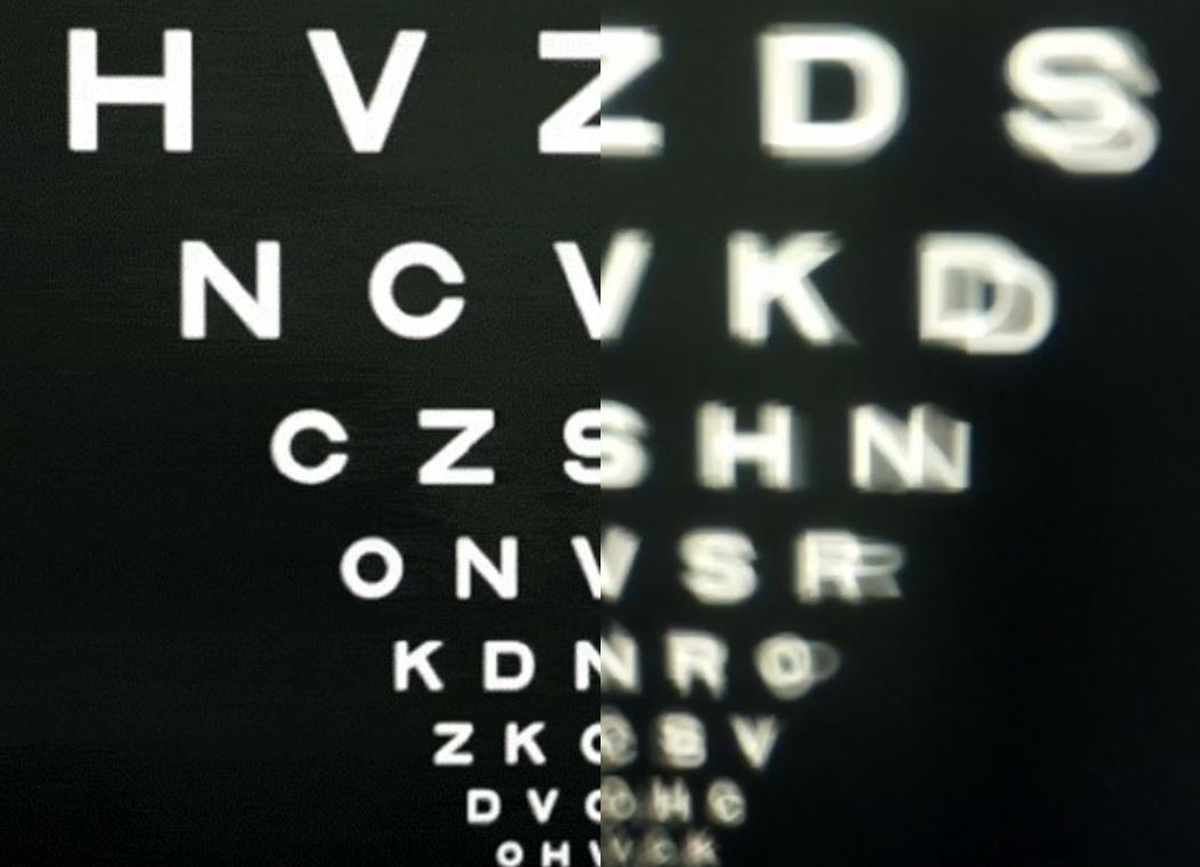
As you can see, with keratoconus, text on a sight chart appears blurred and scattered, with irregular light intensity. The condition affects as many as one in 450 people and is particularly prevalent in certain parts of the world, such as the Middle East. At CC we have several staff members with keratoconus. This was the inspiration for our project, called Kera, launched in November 2023. Our hope is that our findings will enable better and more effective treatments to be offered worldwide.
Patients diagnosed with keratoconus can have surgery, called corneal cross-linking, which strengthens the cornea, preventing further vision degradation. Vision correction is then usually achieved through Rigid Gas Permeable (RGP) contact lenses. These are the treatments I have received, and which have helped to stabilise my affected eye. But in the developing world, keratoconus can go undiagnosed and untreated, causing severe sight problems. Even when diagnosed, the options of surgery and expensive contact lenses are often not available or feasible.
To determine the best treatment for keratoconus, the patient’s cornea needs to be benchmarked to see if there is increasing deterioration or if the eye is stable. However, even in the developed world it is often difficult for an ophthalmologist to ascertain exactly what a patient can and cannot see. This is because the combination of myopia and astigmatism in keratoconus is hard for a patient to put into words.
These difficulties can be intensified if, for example, the patient is non-verbal or there is a language barrier between patient and ophthalmologist. Keratoconus is also challenging to diagnose early for patients with only one affected eye, as the brain adapts to the condition by prioritising the image from the healthier of the two eyes, meaning it takes longer for a patient to realise their vision is compromised.
3D digital cornea reconstruction
What was needed, we decided, was a better way to assess a patient’s visual acuity. It was clear that a hugely helpful step forward would be to create an accurate 3D digital model of the patient’s cornea, so that changes could be tracked. We used topography thickness and elevation scans from a real keratoconus patient to create a full 3D digital reconstruction of their cornea.
We worked in close collaboration with optics experts Luximprint to create a keratoconic lens. Luximprint engineered a novel hybrid additive-subtractive manufacturing process specifically to capture the minute imperfections of a keratoconic cornea. The result was a lens that is perfectly imperfect, covered with the exact flaws that keratoconus damage will cause. We are now using this lens as a keratoconic camera, showing exactly how a person with this condition experiences sight.
We believe the potential for this in practical terms is hugely exciting. While the lens is a tool to communicate the problem more generally, the obvious next step would be to integrate optical simulation into current diagnostics software so they can be readily used by ophthalmologists in clinics worldwide. The scanner could produce a digital reconstruction of a patient’s vision to record any deterioration, but more importantly, provide a meaningful measure of the impact of the deterioration.
The good news is that we are not far away at all from being able to achieve this. We have already generated a 3D model from 2D scan data to demonstrate the principle. Topography scanners already generate this data to a high degree of accuracy.
We feel now that the opportunity for this to make a real difference to keratoconus patients is within reach. If you’d like to discuss keratoconus diagnosis, treatment and therapy further, then please do get in touch so we can continue the conversation.
If you’d like to find out more about keratoconus, here are some useful references: